They are two little charming heroines: When Emma and Ana romp gleefully around the living room, look at their toys with curiosity, or crawl at lightning speed on their knees across the room and make it acoustically known when something is not okay, you would think you were in a totally normal nursery somewhere in Switzerland. If you take a closer look, however, you will see that the two happy children are connected to two colorful bags via white spiral cables that peek out from underneath their clothes. These are the infusion lines leading to the infusion pumps and bags that supply the nutrient solutions for the parenteral nutrition that the two children have needed ever since they were born.
(Published: February 2019)
Parenteral nutrition becomes necessary when a person’s stomach or intestines cannot perform their designated tasks flawlessly, for example due to an operation or a disease. The special liquidized nutrition and the fitting device for administering it are designed to bypass the usual process of digestion and supply the patient with all necessary nutrients such as amino acids, lipids, minerals, and vitamins.
How long these administering processes take depends on the individual case of the patient – Ana needs infusions 18 hours a day and Emma 21 hours a day. Therefore, the parenteral nutrition has to be administered overnight while they are asleep and for several hours during the day. Portable infusion pumps and a backpack system ensure as much freedom of movement as possible for the children. Remarkably, the two see their particular circumstances and all the resulting implications as something totally normal. Their mothers preparing the infusions in the evening before they go to bed, connecting the infusions to the backpacks, the occasional beep the infusion pumps make when an infusion tube gets blocked, or the cleaning of the catheter are all part of their daily rituals. Ana is already able to put her backpack on by herself.
Even interaction with siblings and other children is per the customary rules of a child’s world, be it playing roughly or, through Emma’s masterful charm offensive, getting a boy to wear her backpack, for example. For Ana, going for walks together with her parents and the family dog Aiva is always a special event. Provided the catheter is sufficiently protected, the girls are able to go swimming and splash around, something which creates lots of happy moments, particularly in the summer months out in the garden. Despite their parenteral nutrition, eating and drinking together at the family table allows them to feel part of the family unit and to enjoy their favorite meal.
Ana and Emma’s families got to know each other through the pediatric clinic and have remained on close terms with each other ever since. In addition to the social side of things, the practical tips and mutual exchange of experience are invaluable as far as daily caregiving tasks are concerned. Being accurate throughout the overall treatment and maintaining high levels of hygiene are basic prerequisites for successful and safe parenteral nutrition at home. Both families perform these challenging tasks unfailingly. A specialized outpatient care organization (Kinderspitex) is on hand to provide assistance when needed. At the pediatric clinic, the children are examined and have various lab tests done every month.
The employees in the FresuCare department of Fresenius Kabi in Switzerland are in charge of planning and organizing the supply of nutrient solutions and all of the devices needed for providing pediatric patients with parenteral nutrition at home. Our FresuCare colleagues identify the individual needs of the patients at their home and act as a go-between between families, the pediatric clinic, and the logistics department of Fresenius Kabi. In-house staffs process the families’ online orders, arrange deliveries, and lay the administrative foundations for the direct settlement of costs with the insurers. The FresuCare organization of Fresenius Kabi Switzerland has been able to expertly provide patients with comprehensive clinical nutrition at home for over 25 years, thereby creating significant value for chronically and critically ill patients.
Ana and Emma’s parents especially value the fact that, by being well prepared, the whole family can even go on long journeys and, as a result, are also able to go and see relatives who live far away or visit holiday destinations.
Contact
Fresenius Kabi AG
Else-Kröner-Str. 1
61352 Bad Homburg
Germany
T: +49 6172 686-0
communication@fresenius-kabi.com
A car rattles as it turns the corner. It pushes and weaves its way through the streets of downtown Frankfurt – passing bicycles, pedestrians and horse-drawn carriages. The year is 1912. The car belongs to the Hirsch Pharmacy, one of the oldest apothecaries in the city. And the pharmacy head is Dr. Eduard Fresenius.
Stored in the trunk of the car are various preparations for treatment of skin conditions and colds, as well as sterile solutions for injection. The driver is on his way to sanitariums located on the outskirts of Frankfurt. He makes regular deliveries of Hirsch Pharmacy products to the spas. Pedestrians watch as the car goes by. This is an age when traffic on the streets is characterized by horse-drawn conveyances and bicycles – the car draws attention. Nevertheless Eduard Fresenius invests in the new technology as soon as he takes over the pharmacy from this father. Speedy delivery of pharmaceuticals to patients is a priority for him.
The Hirsch Pharmacy has a long tradition: Its history can be traced back to the 15th Century. The Fresenius family becomes the owners in the 1870s. When Eduard Fresenius takes charge, he has big plans. In 1912 he founds “Dr. Eduard Fresenius chemisch-pharmazeutische Industrie,” in a back room of the pharmaceutical wholesaler. This lays the foundation for today’s healthcare group. A modest pharmaceutical company is born out of the pharmacy laboratory.
Solutions made from the purest distilled water are a specialty of Eduard Fresenius. The quick success of the company also is due to the numerous collaborations that Eduard Fresenius enters into with well known physicians. For Nobel Prize winner Paul Ehrlich, Fresenius develops the “Injectio Fresenius” solvent used in his syphilis cure. Under the name Ampuwa, an abbreviation for ampule water, the solvent to this day is part of the Fresenius inventory."A pharmacy today? we need to expand it or add something new to it." (Dr. Eduard Fresenius)
Eduard Fresenius runs the pharmacy in Frankfurt until 1934, when he relocates company headquarters to Bad Homburg. The company founder is full of ideas on how to gain recognition for his company. Often he is ahead of his time with these ideas. Early in the 1930s he begins distributing a Hirsch Pharmacy magazine for customers. A few years later he opens a diet pavilion in Bad Homburg. During summer months guests consume fresh fruit and vegetable juices. Fresenius employees also prepare special drinks for diet patients based on doctors’ prescriptions. Particularly popular were the milk mix drinks, an early form of the milkshake.
Realizing great ideas is expensive. In financial matters, Eduard Fresenius is unlucky. And the years to come are challenging ones for the businessman. During the Second World War he loses contact with a lot of important business partners. He does not join the Nazi party. Supplying the German army with medications like the Freka frostbite cream helps for a time to maintain company production.
The end of the war finds Eduard Fresenius standing before the rubble that was his existence: Allied bombs have completely destroyed the Hirsch Pharmacy. Raw material shortages make production in Bad Homburg impossible. In the midst of reorganizing the company, Dr. Fresenius dies suddenly in 1946. He names his foster daughter, Else Kröner, née Fernau, as benefactor of his estate.
Just 26 years old, she inherits the Hirsch Pharmacy and the leadership of the company. As a newly licensed pharmacist, Else Kröner knows her way around pharmaceutics, but when it comes to business management she soon reaches her limits. She obtains the needed skills by attending evening classes at a private business school in Frankfurt. She spends nearly 12 hours a day in the company and doggedly works to rebuild the firm during difficult years. Her efforts earn her a great deal of respect and admiration among the staff. She eventually turns over running the Hirsch Pharmacy to a fellow pharmacist. Her main focus now is running the company in Bad Homburg. With a lot of effort, she and her eventual husband, Hans Kröner, develop Fresenius over the following years into a global healthcare group.
Else and Hans Kröner realize they can only keep the company going if they succeed in growing with new ideas. With their employees, they begin searching for new horizons – and soon find one. Since the early days, the expertise of the company has been infusion solutions. Over the next years Fresenius continuously expands its product range, developing new nutrition- and volume replacement solutions such as Generika, which are administered by infusion. The company does more than develop its solutions, it also improves their packaging. Into the 1960s infusion solutions are still stored in glass bottles. Fresenius succeeds in developing special plastic bags and bottles. These are easy to handle, and break proof plastic containers become an immediate market success.
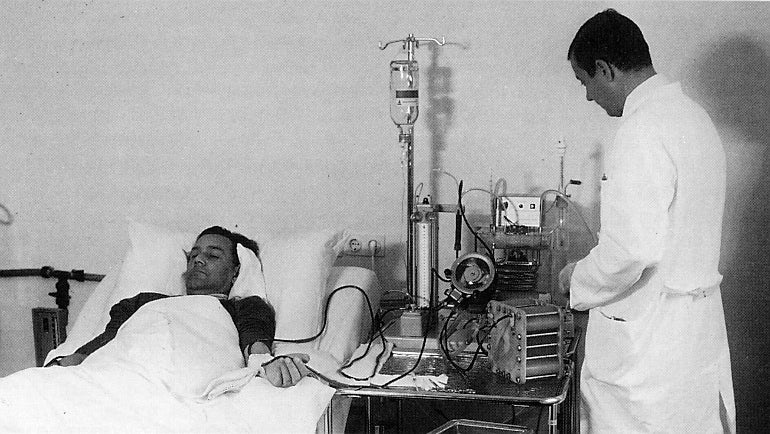
As a medium-sized company producing solutions for dialysis, Fresenius first comes into contact with dialyzers in the 1960s. Dialyzers are blood filters used during a dialysis treatment of patients with chronic kidney failure to purify their blood. This treatment is life saving for kidney patients – but at the time it is very laborious and expensive. Only a few patients can be treated. Through media reports, Fresenius learns of the desperate situation facing many kidney patients, and begins to import American dialysis machines. As they maintain the machines, Fresenius workers gain technical know-how. In the 1970s the company develops its first dialysis machines in a newly acquired plant in Schweinfurt. Constant advancements in materials and technology over the next years enable the company to continue improving dialysis treatment for kidney patients. Fresenius in the 1980s succeeds in developing a capillary made from polysulfone that purifies blood almost as efficiently as a human kidney. To this day blood filters made from this material are the standard in dialysis.
Numerous strategic acquisitions are a hallmark of the next years: 1996 brings the merger of the Fresenius dialysis unit with American dialysis provider National Medical Care to form a new division, Fresenius Medical Care. As a result Fresenius becomes one of the world’s largest providers of dialysis services. In the same year, Fresenius acquires a majority stake in the hospital services provider VAMED AG. Originally founded to plan and build the Vienna General Hospital, VAMED becomes a new business leg for the healthcare group. Acquisition in 1999 of the international infusion business of Pharmacia & Upjohn leads to creation of the business unit Fresenius Kabi.
There are more acquisitions around the world, through which the company also enters the US pharmaceuticals market and assumes a leading role in the global market for generic IV drugs. In 2005, Fresenius takes over the private hospital chain HELIOS Kliniken GmbH and fuses it with Wittgensteiner Kliniken, which it acquired in 2001. This creates the Fresenius Helios division. Fresenius Helios in 2013 acquires 41 hospitals from Rhön-Kliniken, making it the largest hospital operator in Germany.
Hardly any European company in past years has been able to match the dynamic growth of Fresenius. Currently more than 300,000 employees around the world work for the healthcare group. What began as a small pharmacy laboratory is today a leading global healthcare group with a presence in more than 80 countries. The small family operation that Dr. Eduard Fresenius led until his death is different from today’s company in many respects. However the fundamental values of our company are unchanged. To preserve lives and improve the quality of life for sick people has been our motivation for more than 100 years. “Forward thinking healthcare,” symbolizes what we want in the future: constant improvements in medicine for more and more people.
100 Years of Fresenius
Fresenius has been working for over 100 years to improve the lives of seriously ill people around the world. This film, made on the occasion of the company's Centennial in 2012, tells the company's history through the stories of people who have been helped and are still being helped by Fresenius.
The COVID-19 pandemic also presents Fresenius with unprecedented challenges, and our company is doing everything it can to continue providing the best possible care to our patients worldwide. We are not only making every effort to maintain the production and distribution of our products, which are often vital, but to adapt to the new situation and, as far as possible, expand. Our highest priority is the health and safety of patients, caregivers and our own employees.
On this page we are listing a few examples of our activities during the coronavirus crisis. Please keep in mind that this only represents a small selection of our current activities, and that the situation can change at any moment. (Updated: April 30, 2020).
Helios, Germany’s largest private hospital operator and a part of the Fresenius Group, is postponing surgical procedures when medically justifiable and thereby expanding its capacity to care for COVID-19 patients. In addition, the company has increased the number of intensive beds in its hospital network by two-thirds, from 900 to more than 1,500. For this purpose, material reserves are being mobilized and intermediate care beds as well as operating rooms are being equipped and modified with preinstalled ventilation systems.
In order to utilize this additional capacity as effectively as possible, Helios Germany has adjusted some work shifts and taken precautions to send professionals where they are needed most within the company’s hospital network. In addition, several Helios hospitals have admitted COVID-19 patients from Italy in order to help relieve hospitals there. To obtain and secure important data for research into SARS-CoV 2, Helios has established a multi-center COVID-19 register.

In Spain, where conditions are especially strained, Quirónsalud, the country’s largest private hospital operator and also a part of Fresenius Helios, is fully supporting the Spanish government’s efforts to battle the COVID-19 pandemic with all available resources. Quirónsalud increased the number of intensive care beds on short notice. The company is also making every effort to continue providing care for all other patients who urgently need medical support for cases such as chemotherapy and childbirth, as well as emergencies.
"Our employees are all doing extraordinary things. Even at this very difficult time they are still there for our patients."
Thanks to employees’ extraordinary commitment, all Quirónsalud hospitals are successfully maintaining operations despite the high increase in patients with suspected and confirmed cases of the coronavirus. Furthermore, Quirónsalud has succeeded thus far in ensuring that all its hospitals are well-stocked with important medical supplies, despite the sharp increase in demand. And teams of Helios doctors and nurses have already travelled from Germany to Spain to aid their Quirónsalud colleagues.

In Austria, Fresenius Vamed is now using resources from its rehabilitation facilities and clinics to help relieve acute care hospitals. For the time being, the only rehabilitation areas to continue operating will be those where patients urgently need treatment and care, or those that treat patients who would otherwise require acute care. In this regard, the company is also in ongoing contact with healthcare authorities in Germany and Switzerland.
Fresenius Medical Care has further strengthened the existing safety and hygienic standards of its roughly 4,000 dialysis centers worldwide, and taken extensive precautions to ensure patients can continue to receive their lifesaving dialysis treatment. In the United States, Fresenius Medical Care has teamed up with other dialysis providers to create joint capacities for providing isolated treatment of dialysis patients who are infected or may be infected with COVID-19. Furthermore, the company is making 150 additional dialysis machines available to U.S. hospitals for the emergency treatment of COVID-19 patients
The company is also resolutely working to maintain the manufacture and distribution of products for dialysis and extracorporeal therapies. Xenios, a subsidiary of Fresenius Medical Care, has considerably expanded its capacity to produce Novalung, a heart and lung support system for the treatment of acute respiratory or cardiopulmonary failure, and in February delivered a large number of these devices to Wuhan, China, a city hit hard by the pandemic. In Poland, Fresenius Medical Care is making devices for acute dialysis available to hospitals free of charge.
Fresenius Kabi is responding to the significant increase in worldwide demand for essential drugs for the treatment of COVID-19 patients, especially medicines used for sedation such as Propofol and pain management drugs. The company is maximizing supply with all compatible manufacturing capacity now dedicated to these vital drugs. Fresenius Kabi has made significant, future-oriented investments in recent years into both automation and capacity in its manufacturing facilities; these are now enabling treatment for more patients worldwide. Moreover, the company commits itself to keeping prices for essential drugs for COVID-19 patients stable during the pandemic.
In China, Fresenius Kabi was able to bring manufacturing back up to the normal level. Despite some restrictions due to the COVID-19 pandemic and quarantine measures, it has not experienced any interruption in production. This means Fresenius Kabi is still in a position to provide the public with important pharmaceutical and medical products.
Our Chief Executive Officer, Stephan Sturm, thanks the employees for their exceptional dedication in this crisis: “You are all doing extraordinary things: At this very difficult time you are still there for our patients, and sometimes even seem to do the impossible. I can only express, once again, my most sincere thanks. You are Fresenius!”

This friendly golden retriever has been bringing fun, energy and affection into the daily routine of the hospital. Along with his owner Simone Siemke, a family and children’s nurse , Paul supports the medical treatment on the children’s psychosomatics, geriatrics and palliative care wards by coming in and lifting patients’ spirits two or three times every week.
(Published: January 2019)
“On the children’s ward, the little ones can give Paul commands, teach him tricks or give him a reward,” said Siemke. “Some of the children are very shy and lack self-confidence, but when they’re playing with the dog they forget that, and really come out of their shells.” For the older patients, and those suffering from dementia, part of Paul’s training was to learn simple cognitive and motor-function exercises that he can “play” when he goes into the geriatrics ward.

Dogs are proven to have a positive effect on the mood and morale of all kinds of people. A dog doesn’t prejudge anyone, shows affection without expecting anything, and makes an outstanding companion. In particular, a trained therapy dog like Paul can often help ill people to rediscover feelings of happiness, affection and responsibility. Treatments that incorporate the use of therapy dogs can bring improvement in patients suffering from a wide range of mental and physical illnesses; the only precondition is that the individual patient is not allergic to the animals or in any way afraid of them, and agrees to the visits.
Paul’s most challenging assignment so far? “Right at the start a patient in the palliative care ward asked if she could pet a dog one more time ,” Siemke said. “Oftentimes what is needed is Paul’s mobility, but this time it was his very calm and peaceful temper. He just laid quietly on the patient’s bed for half an hour and let her stroke him. It was very warm in the room, and that was the hardest thing for him, but he handled it just great.”
Life in the hospital is not all fun and relaxation for Paul – in fact, it’s sometimes a very difficult job, both physically and emotionally. Like a human employee, he has a contract, which stipulates how often and for how long he should work and when he is free to just be a regular dog. Away from the hospital he can let loose with his full energy – Paul is only two-and-a-half years old – while playing with other dogs, or enjoying long walks with Siemke.
A therapy dog must be very carefully selected and trained. “Generally, all breeds can work as therapy dogs – the only important factors are that they have no potential for aggression and get along well with their owners,” said Siemke. Along with Paul, she completed a 20-month course of training. For Siemke, it included the practical and theoretical aspects of handling and supervising a therapy dog. For Paul, the emphasis was on resistance to stress, patience and obedience.
Therapy dogs are used most commonly in kindergartens and schools, psychiatric hospitals and, occasionally, prisons and other correctional facilities. In Germany, at least, they are being used so far in only a handful of hospitals, and Paul is the first in the Hildesheim region.
Bringing animals into hospitals is generally prohibited for reasons of hygiene, and allowing a therapy dog inside the Helios Hospital Hildesheim is an absolute exception made only under very clear hygienic guidelines and with very strict limitations. This means Paul is allowed to use only a few corridors and stairways, which are cleaned immediately after he passes.
Paul must also undergo veterinary testing and be regularly inoculated, dewormed, bathed and brushed. Before and after each human contact with him, hands and surfaces are disinfected – for the safety of both the patients and their much-loved canine friend.
Contact
Helios Kliniken GmbH
Friedrichstr. 136
10117 Berlin
Germany
T +49 30 521 321-0
Cancer remains one of the greatest challenges facing healthcare systems worldwide. One in every six people dies of this disease, making it the world’s second leading cause of death.
(Published: July 2018)
Yet one of the most modern weapons in the battle against cancer is almost inconceivably tiny, measuring less than one millionth of a millionth of a millimeter across: the proton. In 2020, Quirónsalud, the Spanish hospital group of Fresenius Helios, is planning to open Spain’s first proton beam therapy center.
One of the most advanced cancer treatments, proton beam therapy works by radiating the tumor with positively charged hydrogen atoms, and has major advantages over traditional radiation therapy: The proton beam is narrower, and can be more precisely targeted, which reduces or even eliminates radiation exposure to the surrounding, healthy tissue. As a result, a significantly higher dose can be targeted directly at the tumor, even as the overall amount of radiation used – and the accompanying side effects – are reduced. This makes proton beam therapy especially beneficial for children.
Proton beam therapy has major advantages over traditional radiation therapy.

The secret is in the nature of the proton itself. X-ray radiation, the most commonly used form of radiation therapy, permeates the entire body and its energy decreases exponentially. The initial dose, therefore, must be especially high in order to ensure it still has enough strength to destroy cancer cells when it reaches the tumor. On the way there, and after, it can damage healthy tissue. But because protons only release energy at the end of their trajectories, their impact can be directed to the millimeter.
There are currently only about 20 proton beam therapy centers in Europe, including in Germany, France and Italy. The new Quirónsalud proton beam therapy center, which was built in Madrid, has required an investment of about €40 million.
Quirónsalud has opted for the Proteus One, a unique proton beam therapy system which, unlike others systems, allows all the technology necessary for treatment to be grouped together in one multifunctional room. It includes a tumor-scanning system to help doctors determine the optimal dose for each part of the body being treated, as well as a state-of-the-art imaging systems. And Proteus One can rotate 360 degrees, to direct the beam from any desired angle.
“The investment in building a proton beam therapy center shows how we are continuously seeking better treatment options for our patients,” said Dr. Leticia Moral, General Director for Assistance and Quality at Quirónsalud. “This new equipment and technology will not only enable us to treat cancer patients very effectively and with minimal side effects, but will aid us in researching new types of treatment.”
6 a.m.: The smell of tea wafts through the nurses’ station where a dozen women, steaming mugs in hand, are gathered. The handover from the night shift to the day shift on the Neonatology ward starts on schedule. After everyone is updated, Head Nurse Ines Niemann assigns nurses to the different care rooms. There the shift handover continues in smaller teams: from incubator to incubator, from crib to crib.
(Published: December 2016)
The 22 “beds” on the ward are spread over seven rooms, connected by a long corridor painted in a waterworld theme. Vividly patterned fish, corals, boats, lighthouses and beaches bring brightness and color into a place where they sometimes seem to be in short supply. More than 400 babies born prematurely or with illnesses are treated annually in the Neonatology ward at the HELIOS hospital in Schwerin, a northern German city between Hamburg and Berlin. The ward has four Intensive Care rooms, each with space for three incubators, as well as three Intensive Monitoring rooms with four heated beds in each. There are also three “rooming-in” rooms – called ‘Shark,’ ‘Seahorse’ and ‘Whale’ – with two beds each so that mothers can be with their newborns around the clock.

Babies born before the mother’s 37th week of pregnancy are classified as premature but, as Chief Physician Olaf Kannt explains, “not all children born before the 37th week are in the same danger. The more premature the child is, the greater the challenges in treatment and the higher the risk of complications.” Among them: An overburdened intestine and the inability to take nourishment or breathe without assistance.
All of these complications increase the danger of cerebral hemorrhages, Dr. Kannt explains. “Because those are so difficult to treat, we do everything we can to prevent them.” The specific preventive measures to be taken by the staff are included on a special list prepared by HELIOS. In this document, “minimal handling” is the key term in connection with “preemies,” who must always be handled as delicately as possible and only taken from, or placed back in their incubators or heated beds with extreme care.
The Intensive Care rooms are kept very warm – about 26 degrees Celsius, or 79 degrees Fahrenheit. Medical devices and hi-tech incubators, along with all the hoses, cables and monitors connected to them dominate the room where Nurse Nicole, 39, is caring for Mattes and Emil. She feeds and changes the twins, who were born when their mother was only 28 weeks pregnant, takes their temperatures and administers their medications. They are also turned over regularly, because pressure sores can easily develop on their highly sensitive skin.
Once every shift, Nurse Nicole measures the babies’ blood pressure, and once a week – today is the day – takes blood samples. “We do that first thing in the morning so that the results are available when the doctors make their morning round,” says the nurse. With a practiced technique she takes gentle hold of a tiny heel, carefully punctures a miniscule hole into it and draws a small quantity of blood into a tube. It will be tested to determine the acid-base balance, which will tell if the infusion therapy needs to be adjusted.

8 a.m.: Dr. Kannt starts the morning round, this time accompanied by an unusually large group of doctors and nurses: Once a week, the Neonatology and Obstetrics teams jointly do the round to discuss the status of the babies in the Neonatology ward. In one of the incubators lies Freja. She was born in the 36th week, so the gestation period is less a concern than the fact that she was born with an intestinal obstruction. As a newborn she had to undergo two operations. Today, the visiting doctors decide Freja’s stitches can be removed.
10 a.m.: The first mothers arrive. One of them is Xenia Dräger, Mattes und Emil’s mother. Ever since she has been allowed to care for her sons, she has been staying in a rooming-in room and from 10 a.m. until midnight washes and changes them, keeps a watchful eye as they sleep, and talks to them. The twins lie in heated, transparent plexiglas incubators, fed through tubes that enter the nose and continue down to the stomach. The room is quiet, except for the peeping from monitors and other assembled medical equipment.During the daytime, parents take the lead in care, with nurses always nearby, ready to advise them or take over if necessary.

Because their lungs are not yet developed enough for the twins to breathe unassisted, they are attached to respirators. Their tiny faces are almost invisible behind the breathing masks, which make them look almost like miniature skin divers. Electrodes attached to their chests and feet monitor circulation. One suddenly sounds an alarm: Emil’s breathing has been interrupted and his heart rate is dropping. Xenia, who is standing beside the incubator, has been taught by a Neonatology nurse how to respond: she gently massages her son’s chest and presses against his feet. He starts to breathe regularly again, and the monitor goes quiet.
“Mattes does it very nicely, but Emil unfortunately still has frequent interruptions in his breathing,” Xenia says, gently stroking his head. “He still has to learn that.” Twice daily, the twins lay at her breast for one to two hours for so-called “kangarooing.” The term might be humorous, but the practice has a serious purpose: Studies show that it quiets the babies, making both breathing and the heart rate more stable.
2 p.m.: Arriving for the late shift is Nurse Konstanze, who no longer works in the Intensive Care rooms. “Since I became a mother it has been difficult for me to look after the tiny little ones who are struggling for life,” she says. “I feel better here in the Intensive Monitoring rooms.” In these rooms it is the babies’ own rhythms that dictate the care: lying in their warm beds, they are generally monitored only through a small cuff wrapped around a foot.
During the daytime, parents take the lead in care, with nurses always nearby, ready to advise them or take over if necessary. “A lot of parents are nervous dealing with their children, especially when the kids are still sick,” says Nurse Konstanze. “First and foremost, it’s our job to take away that fear, show them how to handle their kids and make them feel secure about it.”

4 p.m.: It’s cuddling time for newborn Freja and her mother, Lisa Dierenfeld, who announces proudly: “She took my breast for the first time today.” There is both joy and relief in the young mother’s voice. “We knew during my pregnancy that Freja had an intestinal obstruction that ended outside of her stomach. We knew that she would have to undergo surgery right after she was born, and be in the ward for premature babies.”
Freja was delivered by caesarean four weeks early, and what followed was also difficult for her mother. “I couldn’t see my baby until two days after her birth,” Lisa recalls. “All the equipment around her bed, the cables and the monitors; it was a shock – I just cried. On the third day I could take Freja in my arms, and that was the first time I really felt like I had given birth.” But the patience and waiting for her daughter to improve have paid off: Lisa will finally be able to move into a rooming-in room later in the day, and she’s full of confidence.
“I am moving in there and I’ll stay until my daughter and I can go home together,” the young mother declares.

8 p.m.: It’s quiet time until 11 p.m., when the next care round will begin. The only sounds on the ward are the low swooshing of the respirators and the occasional alarm signaling that a baby has forgotten to breathe, which sends the nurses rushing in to massage tiny chests or feet until regular breathing starts again. A member of the night shift team is Nurse Janet, who works in the Intensive Monitoring rooms and now has six babies in her care. The 44-year-old nurse does not realize yet that there will be a seventh before the night is out.
10:30 p.m.: The late shift duty doctor, Senior Physician Christian Güttel, arrives and begins checking on what he should expect overnight. He then takes a close look at all the babies, examining some of them, and turns to Nurse Janet. “In the delivery room there’s a woman in her 34th week,” he says. “Don’t be surprised if we get an addition tonight.” It turns out he’s right: The call comes an hour later and, together, doctor and nurse wheel a mobile incubator out of the Neonatal ward and return a short time later with Robin, who is only minutes old.
Dr. Güttel examines the baby boy – the lack of wrinkles under the soles of the feet and the fingernails that don’t yet reach the fingertips are clear signs of a premature birth. “Every child born before the 37th week of pregnancy comes to Neonatology for monitoring,” he says. “With our knowledge and medical equipment we try here to stimulate development as it is in the mother’s womb. Our kids get all the medical help they need.”
3:30 a.m.: The rest of the night is quiet, and already it’s time for the last care round before the shift ends. Nurse Janet draws charts for the day ahead and fills the infusion and disinfectant dispensers. Someone is making tea so that it will be ready when the colleagues from the day shift arrive.
Contact
Helios Kliniken GmbH
Friedrichstr. 136
10117 Berlin
Germany
T +49 30 521 321-0

8:30 a.m. In the children's operating room of the Leipzig Heart Center, final preparations are underway. Philipp, just nine days old, is already under anesthesia on the operating table in the middle of the room.
(Published: February 2018)
The regular beeping of the ECG and the lines on a monitor indicate that his heart is working normally, and yet Philipp suffers from a very serious congenital heart defect: His pulmonary artery and aorta are transposed, which causes the blood and pulmonary circulation to run in parallel instead of in sequence, as they should. The baby’s body is barely getting enough oxygen, and only surgery can correct this anatomical defect and save his life.

The procedure is challenging, but Philipp is in very good hands. His pediatric cardiac surgeon, Prof. Martin Kostelka, is one of the world’s best. He has performed more than 10,000 operations during his 30-year career, with a 99 percent success rate. The youngest child Prof. Kostelka has operated on was a premature baby born in the 25th week of pregnancy and weighing just 460 grams (a little more than one pound); the oldest “child” was a woman who was 77 when her congenital heart defect was detected.
In an average week, Prof. Kostelka will operate seven times in the children's operating room of the Leipzig Heart Center, assisted by his team of surgical nurses, anesthesiologists, perfusionists, junior doctors and surgical assistants. Among them is Ingrid Conradt, a surgical nurse who has worked at the Leipzig Heart Center for more than 20 years. "We are a very experienced team," she explains. "We can rely on each other 100 percent."
9 a.m. Prof. Kostelka makes an incision in Philipp's chest and opens the rib cage to expose the heart, which is about the size of a walnut. The next step is for the perfusionist to connect a heart-lung machine especially adapted for children. Prof. Kostelka gives brief instructions. Temperature, speed, the flow in the heart-lung machine, pressure … everything must be just right when the machine takes over the work of Philipp's heart to pump blood through his body. Shortly after 10 a.m., with Philipp's heart stopped, Prof. Kostelka's real work begins – the delicate transplanting of tiny coronary arteries and the transposed large vessels so that, when all is done, they will extend from the proper ventricle.

12 noon. While silent concentration dominates the children's operating room, it’s a bit louder two floors down in the electrophysiology (EP) laboratory, where Professor Andreas Bollmann, Chief Physician in the Department of Cardiac Rhythmology, is calling out for 35 watts. "We rhythmology specialists are essentially cardiac electricians," he says with a grin. "We’re able to treat hearts that are beating too fast, too irregularly or too slowly, by using ablations or by fitting defibrillators and pacemakers, which offer a great chance of healing."
Lying before Prof. Bollmann is Guenther K., who suffers from atrial fibrillation, one of the most common cardiac arrhythmias. The doctor threads a catheter with an electrode into the 67-year-old patient's heart via an opening in the groin, which allows the points that are conducting the abnormal stimulus to be gradually neutralized. On a huge screen, he can see not only the lines of the ECG and an X-ray image of the heart but also a bright, almost amoeba-like 3D structure. "That is the left atrium with the pulmonary veins draining into it. With the help of this exact representation, we work out the precise route above the sites to be neutralized," Prof. Bollmann explains. While he guides the catheter, his team stands at what resembles a control center consisting of various monitors and apparatus. They provide the required electrical impulses, according to his instructions, measure parameters, and check imaging.

"We not only have the world's largest EP lab here, we also have the most innovative technology and imaging in this field," Prof. Bollmann says. In 2015, Fresenius Helios invested more than €5 million in the Leipzig Heart Center’s EP labs.
But it is not just modernity and innovation that make the heart center in Leipzig, a major city in eastern Germany with a population of 560,000, internationally attractive: Ongoing research in all fields of cardiovascular medicine attracts doctors from all over the world, who receive advanced training here or transfer permanently to the Leipzig Heart Center. In the Department of Cardiac Rhythmology alone there are doctors representing eight nationalities. Overall, people from more than 40 countries work at the Leipzig Heart Center.
5:30 p.m. Back in the pediatric intensive care unit, Philipp has survived the complex surgery. The four hours originally scheduled for the baby’s operation turned into nearly eight, and Prof. Kostelka looks tired, but happy. "Sometimes during an operation, the situation turns out to be much more complex than first assumed,” the surgeon says. “Then you have to deviate from your routine, react and find solutions. That’s how it was with Philipp. Due to an anatomical abnormality of the coronary arteries we had to start again three times, which meant that we also stopped the heart three times. As you can imagine this was a tremendous strain for the little boy.”
“However,” adds Prof. Kostelka, smiling, “we managed it, and now I am really happy and optimistic."
Only three weeks later, Philipp is well enough to leave the hospital with his mother. The infant is doing well, and can now begin to enjoy a healthy life with his family.
Pictures: © Thomas Oberländer, Helios
Contact
Helios Kliniken GmbH
Friedrichstr. 136
10117 Berlin
Germany
T +49 30 521 321-0

Nathalie Neubert, who is pursuing a cooperative university program in International Business, and Raphael Boos, an apprentice in Mechatronics, asked Dr. Krick about his career, the development of Fresenius and his ideas about the best subject to study – and received direct, spontaneous and to-the-point answers.
(Published: January 2018)
Nathalie Neubert: Welcome, Dr. Krick. It is our pleasure to be conducting this interview with you today. You have been with Fresenius for more than 40 years. When you started here, the company had barely 1,000 employees, most of them in Germany. Today there are nearly 300,000 spread around the world in more than 100 countries. What do you think has been the biggest change over the years? Or perhaps, what has remained unchanged?
Dr. Gerd Krick: This is not an easy question. What has remained the same is the job. The work today is every bit the same as the work we used to perform. What has changed is that, when you head a company or hold a higher position, it is no longer possible to know every employee. They are now so numerous that you don’t even know all those in leading positions. In the old days you knew everybody. I used to walk through the filling station and would know the person operating the filling machine. Those days are over.
Raphael Boos: It used to be common for an employee to stay with one company for a whole career. Nowadays, it is very common for an employee to switch jobs frequently. You are somebody who has spent an impressive 40 years or more at the same company. Was there a time in your career when you thought you should try something different elsewhere?
Dr. Gerd Krick: Not really, because the work was so interesting that I never thought about going anywhere else. The company grew, and continues to grow, which made the challenges so interesting that nothing would have been gained by switching to another employer. Of course, it’s only natural to check the newspaper occasionally. But when comparing opportunities, it became clear that this field was the right one. It is a great advantage for us to be in health care and, there should be no doubt about this, anyone in health care who is not growing is doing something wrong.
Raphael Boos: You played a key role in shaping Fresenius. But the question occurs to me: To what extent did Fresenius play a role in shaping you?
Dr. Gerd Krick: I don’t have an answer for that. I am what I am. The key thing that I would say to those who are just starting at a company is: Remain true to your ideals. I have never compromised my standards. That’s why I can’t really say that Fresenius has changed me. I am what I am.
Raphael Boos: That’s a very good trait to have. As a trainee mechatronic engineer, I would like to delve a bit deeper into the aspects of engineering, and ask: What is more important to an engineer; technical expertise or creativity?
Dr. Gerd Krick: Basically, creativity. You have to say to yourself: What do I need to make something better? And the answer is: To make something really better, you must be creative. I think creativity plays a much greater role in this than pure technical expertise.

Nathalie Neubert: Although you hold a doctorate in engineering, you have long been a part of company leadership. What advice would you give young people like us, who are also interested in a management role – should we pursue studies in engineering, or classic business administration?
Dr. Gerd Krick: At the risk of sounding superior, I would very seriously advise studying engineering. This is something in life you will not be able to get anywhere else, whereas making sales and keeping books can be learned later in the course of a business career. The skills gained from studying business administration are easier to obtain in daily life than engineering expertise.
Raphael Boos: If you wanted to develop another new product tomorrow, what would interest you the most?
Dr. Gerd Krick: I would say dialysis is the obvious candidate. The one truly unsolved problem in dialysis is the shunt, meaning the connection from vein to artery. The shunt is a synthetic product. The connection is there to achieve high blood flows. You can’t perform dialysis with low blood flows.
A shunt can break and cause infection – that is a fundamental problem in dialysis. Fresenius Medical Care has just entered into an agreement with Humacyte, which is developing a vascular system that is based on human cells. This is a breakthrough innovation. If I had to decide what I was going to do all over again, this is where I would begin.

Nathalie Neubert: For the past 15 years you have been Chairman of the Supervisory Board. We believe not many people at Fresenius really know what the person in this position actually does, and it certainly is no ordinary job. So, we would like to ask you if you would be so kind as to give us a brief glimpse into your duties.
Dr. Gerd Krick: To do that would take a very long time, but I’ll try to make it brief. With the knowledge gained over the years about products, innovations, markets and “how to sell,” we discuss and evaluate projects submitted by the Management Board.
It is nearly impossible for the Supervisory Board to check all facets of any of these projects. This would necessitate preparing them ourselves. It would require us to conduct our own negotiations. This is beyond the means of a Supervisory Board. This means that what we do is employ knowledge gained in the profession to evaluate and discuss projects with the Management Board. They must supply answers to the questions we raise. This latter point is the most important function. If someone intends to run the business from the Supervisory Board – and I have always said this – then they should stay on the Management Board.
Nathalie Neubert: We have reached the end of our interview. Just one more question: Would you like to use this opportunity to send another key message to Fresenius employees?
Dr. Gerd Krick: The message is very simple: Continue to be successful – and be better than your competitors!
Raphael Boos: Many thanks, Dr. Krick, for this wonderful interview. We wish you all the best in your future endeavors.
Nathalie Neubert: Many thanks for taking the time to talk with us.
Dr. Gerd Krick: It was a pleasure to talk with you. Thanks. I hope that I can be part of the continuing growth for some time yet.
The loud beeping from the monitor pierces the room. The patient's heart rate is accelerating, his breathing is labored, and he is starting to cough. Also, the right side of his face is swollen.
(Published: December 2016)
"Do you have any allergies, Mr. Schönfeld?" the physician asks, bending over and carefully feeling around the patient’s neck. "No allergies," comes the reply, in a slurred voice. But with the patient’s blood pressure dropping rapidly, Nurse Romy Wiessner asks if support should be called in. At a nod from Assistant Physician Dr. Roland Hiersemann she rushes to the telephone, and calls into the handset: "We need backup in the emergency department!”
Wiessner, on returning to the patient's bedside, rolls up his sleeves and inserts an IV cannula. When she withdraws the needle there is a drop of blood on it. Usually, this would be unremarkable, but in this case it is technical ingenuity: Mr. Schönfeld is not made of flesh and blood, after all, but of plastic, wires and electronic components.
In the Simulation Center at HELIOS Hospital Hildesheim in northern Germany, doctors and nursing staff train not on real patients but on high-tech patient simulators – mannequins such as Mr. Schönfeld that look like patients and can talk, breathe and perspire. They have a pulse, and you can take blood samples from them. Sometimes they even cry.
That they react like real patients is in no small part due to Stephan Düsterwald, the center’s medical director, and his team. During each training session they huddle in a small room behind a glass panel and control the patient simulator’s reactions – making the heart beat faster or the eyes blink, for example. "We can simulate life-threatening situations in a realistic environment without harming a patient,” Düsterwald explains. “In these stressful situations here, unlike in real life, mistakes are expressly allowed."
"A little while ago it was only a piece of plastic, but just now it was my patient."
Just as the second team of doctors, headed by Dr. Martin Köhler, arrives, the oxygen level in the blood of the “patient” drops sharply: He is in critical condition. Dr. Hiersemann calls out to check that adrenaline has been given, as ordered, and looks around the room, but no one answers. The other team members busily fetch drugs, attach oxygen and measure blood pressure again, while continually glancing up at the monitor. Still there is no improvement, so the doctors quickly administer an anesthetic and begin an intubation – which proves to be difficult because of the extreme swelling of the throat. As Dr. Köhler carefully inserts the breathing tube into the windpipe, Dr. Hiersemann sets his stethoscope on the patient simulator’s plastic chest, and after a few seconds confirms the tube is in the correct position. The mechanical ventilation is started and the treatment team looks relieved as the blood’s oxygen level starts to increase.
Suddenly, the beeping of the monitoring screen stops and there is silence. Düsterwald and his team enter the room, ending the 15-minute training session. Slowly, the participants start to relax. "It felt completely real," Dr. Köhler says in a tone of near-disbelief, as he instinctively goes to a dispenser and rubs some disinfectant into his hands. "A little while ago it was only a piece of plastic, but just now it was my patient."
Everyone makes mistakes: Every 30 minutes on average when performing routine duties, and much more frequently – as often as twice a minute, according to studies – during more complex, higher-stress tasks.
“Professionals also make mistakes,” says Düsterwald. “We record all the training sessions with a digital audio video system, which enables us to detect even slight irregularities and analyze with the participants how they could have been avoided. And this way we ultimately improve the safety of our patients. Our doctors and nursing staff can draw on a vast wealth of knowledge and experience, and even in the most serious situations the knowledge needed to solve the problem is often in the room. We just need to make sure the right measures are actually carried out on the patient. Communication within the team and with the patient plays an important role, so that is something we focus on during the training sessions."
Afterward, the participants gather for a debriefing and to view a few key scenes from the video. Enough time has passed for them to watch with a good measure of objectivity, and they not only congratulate each other on successful diagnoses but are able to openly make some constructive criticisms. "The handover to the second team of doctors could have been more coordinated," says Bastian Overheu, the Simulation Center’s deputy director. "It was no longer clear who was leading the team. A short break, using the 10-for-10 principle for example, and the situation could have been straightened out."
According to this principle, doctors and nurses should continue to take short breaks – especially when things are hectic – even for as little as 10 seconds every 10 minutes. That is enough time for the physician in charge to announce the treatment plan out loud, ensuring that everyone on the team has the same understanding of the situation, and to ensure that good ideas from the nursing staff do not go unheard.
“Good teams often have, implicitly, the same understanding of a situation,” explains Düsterwald. “They communicate almost without words. Misunderstandings are rare, but they can occur, so it is always good to let colleagues know that you have heard questions or instructions. That is a simple and important safety mechanism that we pass on to all our participants.”
At Fresenius Helios, simulation training for all doctors and nursing staff in higher risk areas, such as intensive care medicine and anesthesia, became mandatory this year. Specialists from emergency medicine, obstetrics and the cardiac catheterization lab undergo regular training. Other concepts are planned for gastroenterology and surgery. All participants take courses conforming to unified standards, and in fully equipped operating and treatment rooms.
More than 600 separate training days are held annually in HELIOS’s simulation centers in Hildesheim and two other German cities, Erfurt and Krefeld. The company has invested a total of about €2 million in the three facilities. A special feature of the Simulation Center in Krefeld is a fully integrated simulation ambulance: to make it as realistic as possible, the “vehicle” has the full original interior and even comes complete with rear and side doors.
Contact
Helios Kliniken GmbH
Friedrichstr. 136
10117 Berlin
Germany
T +49 30 521 321-0

Hygiene in hospitals is essential for the survival of patients, and efforts made by hospitals to ensure high standards of hygiene are enormous. Yet cases of bacteria spreading between patients and hospital wards continue to occur, even in wealthy, technologically advanced countries.
(Published: July 2017)
For example at the HELIOS Hospital Duisburg, in western Germany: This maximum-care facility, a university teaching hospital with more than 1,000 beds and 24 specialist departments, was hit by a wave of infections caused by multiresistant bacteria. Mistakes had been made in hygiene management, plunging the hospital into a crisis. Since then, important lessons have been learned. This article illustrates how improvements have been made and rigorously implemented. Hygiene standards in the hospital are now at their highest level ever.
August 13, 2013, was a perfect summer Saturday in Duisburg, but at HELIOS Hospital Duisburg a storm was raging. “Alarm on spreading bacteria in hospital,” read one headline. Another warned readers of a “skyrocketing increase in MRSA infections” at the hospital. MRSA – methicillin-resistant bacteria – has been identified by the World Health Organization as one of the antibiotic-resistant “superbugs” that pose a huge threat to public health worldwide. The outbreak caused many people to lose confidence in the hospital. The number of patients dropped – and so did the employees’ morale.
An important element in the sustained success has been a regular dialogue between all involved staff.Today, less than four years later, HELIOS Hospital Duisburg has one of the best infection-prevention records in the HELIOS Group, which regularly makes its hygiene data public. For Dr. Holger Raphael, the hospital’s Managing Director since mid-2013, this gives cause for satisfaction but not complacency. “We managed to turn things around that time,” he says. “But preventing infection is a never-ending story, particularly in light of the increase worldwide in antibiotic resistance. Our first priority now is what it always has been: to keep reminding ourselves of what is at stake.”

The storm clouds that burst in 2013 were present before Fresenius Helios acquired the hospital in late 2011. Infections do not increase overnight – most are a result of inefficient organization, poor quality medical care or a lack of knowledge among employees. Further complicating matters, HELIOS Hospital Duisburg has several clinics spread across the city of 490,000 people, an industrial center at the intersection of the Rhine and Ruhr Rivers. This necessitates countless daily “patient transports” between the clinics, and can make it more difficult to share information.
“For a long time there was a lot of uncertainty about how to deal with multi-resistant pathogens,” explained Ankica Gagro, who is now Head Nurse in the Cardiology Department . “There were few uniform standards, so, over time, many departments established their own procedures.” The result was that standards varied from ward to ward, even though the conditions and pathogens were identical. Many employees lacked a channel for communication and access to information.
When the “germ scandal” hit, the integration of the hospital into the HELIOS Group was still incomplete. Improvements in hygiene management had not yet been fully implemented. When the bacteria appeared, the pace of change was accelerated in affected departments: Hospital management and Dr. Natalie Pausner, the new Senior Hospital Hygienist, analyzed and prioritized the problems. Renewed energy was put into carrying out long-established procedures more thoroughly.

“We immediately brought all employees working in areas with close patient contact into the review of the situation and improved our hygiene guidelines,” recalled Dr. Markus Schmitz, Chief Physician for Anesthesiology and the hospital’s Medical Director since early 2013. “The staff then received intensive training. From this point on, a bottle of disinfectant became standard equipment in the pocket of every physician and care employee.”
At the same time, acute problems were recognized and put onto the agenda more quickly. One example was reporting over-use of antibiotics, which can increase bacterial resistance. “That year we also began to extend antibiotic rounds, during which doctors review antibiotic use, to all departments, and to screen all patients for MRSA when they were admitted to hospital,” said Dr. Schmitz. Steps were taken to ensure laboratory results were obtained faster. A weekly internal conference was started where every death in the hospital was discussed with all involved medical personnel. This gave doctors clues on how to better treat similar cases in the future.
An important element in the sustained success on improving hygiene has been a regular dialogue between all involved medical and managerial staff. Doctors Pausner and Schmitz, for example, meet every four weeks and send a monthly report with the hospital’s latest infection data to hospital management and all chief physicians. Among measures launched on their initiative was the introduction in 2015 of short-sleeved shirts for doctors, to prevent transmission of bacteria that can cling to long sleeves.
HELIOS Hospital Duisburg has adopted many more measures to ensure that hygiene standards will continue their steady improvement. The hospital participates in data collection programs organized by a national center and operates an in-house data bank for pathogens, both of which help to pinpoint areas to implement or improve hygiene measures. All hospital wards are better targeting the placement of disinfectants. There is also a standard range of products and techniques for cleansing patients of bacteria. Every specialist department has doctors and nurses responsible for hygiene. An online training module for continuously updating hygiene training and practices has been launched.
“In addition,” said Dr. Pausner, “we flag patients with multiresistant pathogens much more visibly, both in their electronic file and also directly at their bed.” Doctors and their teams regularly update other employees via the intranet and, in acute cases, proceed promptly to the ward. Other hospital staff can make frequent use of the information and share it with colleagues, which helps maintain a focus on hygiene and infection prevention. Constant increased awareness of hygiene issues by hospital staff has probably been the most important and beneficial lesson to have come out of the difficult days of summer 2013, said Dr. Raphael.
Contact
Helios Kliniken GmbH
Friedrichstr. 136
10117 Berlin
Germany
T +49 30 521 321-0