When the spine is operated on, mere millimeters can be critical. For such highly complex procedures, surgeons need sound judgment, precise spatial awareness, the capacity for abstraction – and a skilled pair of hands. Yet by their very nature, humans frequently reach the limits of their abilities. That is why many hospitals have for a long time been using high-resolution three-dimensional images and surgical navigation systems, such as spinal navigation, to perform their work. But all of this is only the start.
The Department of Neurosurgery and the Center for Spine Therapy at Helios Hospital Berlin-Buch have continued to build on their expertise in spinal surgical procedures: Under the direction of chief physician Professor Yu-Mi Ryang, the department has been using augmented reality (AR) in spinal stabilization surgery for the past two years. Berlin-Buch is thus one of the first hospitals in Germany to use AI in neurosurgery for the benefit of patients. The AR technology makes the procedures more precise, less invasive, and also shorter. A look over the shoulder of Prof. Ryang reveals exactly how AR is used here and why this represents an important step into the future.

There is total concentration in the operation room. Prof. Ryang is leaning over her patient. He is suffering from a spinal tumor that has already partially destroyed the bones and is also pressing on the highly sensitive spinal cord. Over the course of the next two to three hours, the surgeon will remove the tumor from the spinal cord and strengthen the area of the spine destabilized by the tumor using a so-called screw and rod system. It should restabilize the spine and, above all else, free the patient from pain. The neurosurgery teams also use such minimally invasive techniques for other indications, combining them with AR technology – in frequently occurring cases of wear and tear of the spine, for example, as well as when repairing fractured vertebrae after an accident or treating osteoporosis.
In purely visual terms, this screw and rod system resembles a railroad track. Firstly, between four and eight, sometimes significantly more, screws are firmly anchored in the “track bed” – i.e. the vertebral bodies. To this end, the screws are attached to so-called towers, which function as a kind of screw extension. Without these towers, the screws would disappear into the depth of the surgical area when inserted. They would no longer be visible to the surgeon and would hardly be accessible through the back muscles.
All of this is preferably performed in a minimally invasive procedure by making small incisions in the skin in order to preserve the tissue and reduce blood loss. Other advantages of this tissue-preserving procedure include a shorter operating time. This is because there is no longer any need for the complex process of detaching the back muscles from the spine, as is the case with open procedures. The patient also suffers less postoperative pain.
Due to the minimally invasive technique, Prof. Ryang may only be able to see a small section of the surgical area with her own eyes, but this is no obstacle thanks to AI. The precise location where the rods have to be inserted and, above all, the required length and curvature, along with the location of other important structures of the spine – such as the spinal cord or the tumor itself – can all be shown to her with the help of augmented reality. The latter also increases the safety of the procedure.

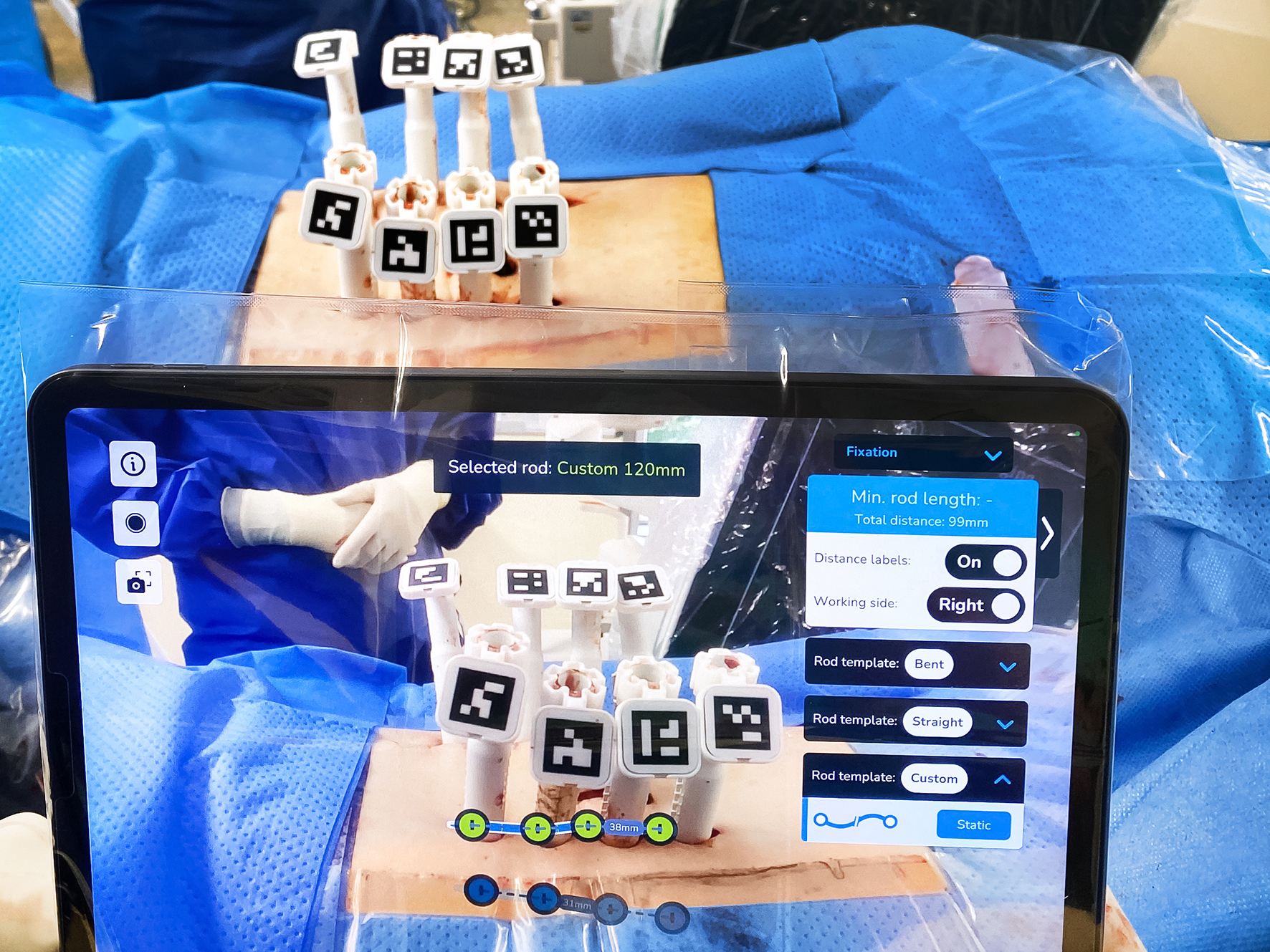
As the operation progresses, things get tricky again: Depending on the curvature of the spine, Prof. Ryang has to shape the titanium rods in advance so that they fit perfectly into the screw heads. Being even a few millimeters out can make a big difference here. In the past, the team relied purely on operative experience and their own judgment when shaping and fitting the rods. “This can be extremely difficult, however, particularly with severe curvatures of the spine,” explains the surgeon. Furthermore, it is relatively time-consuming. This is precisely where AR can now help: “With the aid of augmented reality, we can determine the ideal position, length, and curvature of the rods during the ongoing operation in a matter of minutes and prepare them accordingly.”
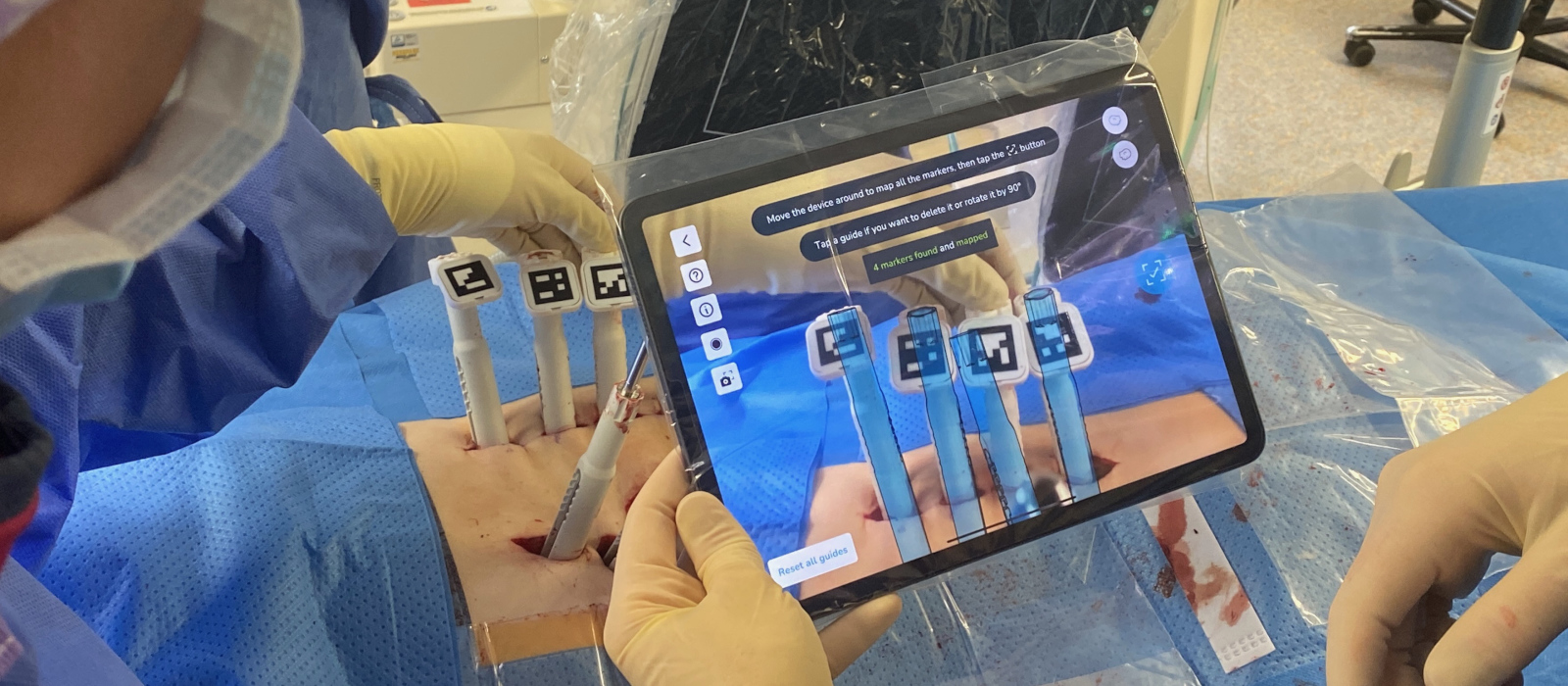
When the term augmented reality (AR) is mentioned, many people tend to think of virtual reality (VR) headsets. In Berlin-Buch, however, the neurosurgery team works with standard tablets equipped with a built-in camera and special software. Dr. Ryang points the tablet camera at the patient’s back. By swiveling the tablet, the surgical area is scanned – and with it the QR codes affixed to the screw tower in advance. The virtual 3D towers and virtual rods then gradually appear on the tablet, which are assigned to the real-time image of the patient. “Changes in position during the procedure are also no problem for me – orientation is guaranteed at all times,” says Prof. Ryang. With the aid of the QR codes, the tablet’s integrated camera can determine the exact position of the inserted screws and the exact length and curvature of the rods. And it can “merge” with the patient’s real-time image as a virtual 3D image. Based on this augmented reality, the surgeon can then use the tablet to create custom rods for each individual patient.
The software works out a kind of template for this, enabling the surgeon to bend the titanium rods into the ideal shape by hand. To allow her to compare, she repeatedly places the rods on the template. In the past, if the rod was not perfectly bent, a screw could be ripped out of its position again after being inserted. The doctor says that this risk is now minimal: “We hope that there will be significantly fewer postoperative complications in the long term, such as a broken rod, a loose screw, or some other material failure. Any of these things would necessitate revision surgery. We also hope that this method will improve the clinical outcome of patients in terms of pain and quality of life.”
The neurosurgery team in Berlin-Buch has been using AR technology for about two years now. At the present time, the interim assessment looks promising: Several studies have shown that it improves operative performance. “Even highly experienced surgeons are not always able to set the ideal curvature radii of the screw and rod systems without augmented reality support,” says Dr. Ryang. “But with the help of AR, practically all surgeons are able to achieve perfect results.”
Yet it gets even better with augmented reality: AR-supported procedures lead to shorter operating times, thereby also reducing the length of time the patient spends under anesthetic. This represents a continuation of the positive trend seen in spinal treatments, with minimally invasive neurosurgical procedures on the back becoming more and more comfortable for the patient.
“Our example from Berlin-Buch shows what it means to bring a medical innovation to patients in a very practical way,” says a delighted Prof. Ryang. “It is not the one major revolution that changes everything overnight. Rather, we combine various innovative solutions to achieve better outcomes for our patients step by step,” says the expert in summary.
Top specialist in neurosurgery
Prof. Yu-Mi Ryang studied at Ruhr University Bochum, where she also gained her doctorate. The Düsseldorf-born physician then worked in the field of neurosurgery at University Hospital RWTH Aachen, where she completed her specialist training. Prof. Ryang attained her professorship at the Klinikum rechts der Isar of the Technical University of Munich and was appointed senior physician and deputy director of the Neurosurgical Department and Polyclinic in 2017. The specialist joined Fresenius Helios in Berlin-Buch in 2019. As chief physician, she heads the Neurosurgical Department as well as the Center for Spine Therapy.
She also holds a number of positions in various national and international professional societies, including the German Society of Neurosurgery, or DGNC, where Prof. Ryang is currently head of the spine section. In addition, she is on the board of the German Spine Society (DWG), where she serves on various commissions and is chairwoman of Module 5 of the DWG’s basic courses. In EUROSPINE, Prof. Ryang is also chairwoman of Module 4, and in AO Spine she is a member of the Technical Commission and the “Fracture, Tumor, Deformity Expert Group.”


