The so-called CAR-T cell therapies are among the most innovative therapy options for malignant blood cancers, for example. They require the patient’s living cells, which are then prepared in a special way using an intricate process. The entire production process for these cell-based therapeutics is extremely complex and logistically challenging, making therapeutic applications expensive and limiting their accessibility:
(Published: November 2024)
Firstly, the patient’s blood cells are removed. The immune cells are then isolated and genetically modified, usually with an engineered virus. They are then expanded – grown to large numbers to be exact – and formulated, thus prepared before being reinfused into the patient. All of this must be carried out in a sterile environment for a batch size of exactly one counter. Because each course of CAR-T cell therapy is individually tailored to each patient – and that is precisely what makes the therapy so special. At present, medical professionals and researchers often need a production period lasting three to six weeks before an individual course of CAR-T therapy is available.
Read more about this in the interview with Chris Wegener, Director, CGT R&D, Research and Advanced Technologies, Transfusion and Cell Therapies Fresenius Kabi USA.
First step toward streamlining: Simple centralization in one production facility
Due to this lengthy and complex production process, the cells are usually produced centrally in one single production facility, not least because highly qualified personnel, the special laboratory equipment, and the necessary infrastructure are all available here. All of this entails major logistical challenges, however, and production bottlenecks can sometimes occur. “And the costs are always high,” explains Chris Wegener. “The resulting therapies thus end up being very expensive overall and practitioners are currently unable to meet the needs of the entire patient population,” he adds.
In order to democratize the treatment and make it accessible to more patients, experts in the cell and gene therapy industry have been working hard for a long time to find new approaches. Their aim is to simplify the process and thus reduce the production costs of CAR-T cell therapy. To be able to do this, however, there needs to be a fundamental change to the way in which CAR-T cells are produced. One of the options for streamlining the process involves further automating the central production. For any such automation to be more efficient, new tools also need to be developed and made available. And it is precisely at this point in the development history that the engineering teams at Fresenius got down to work.

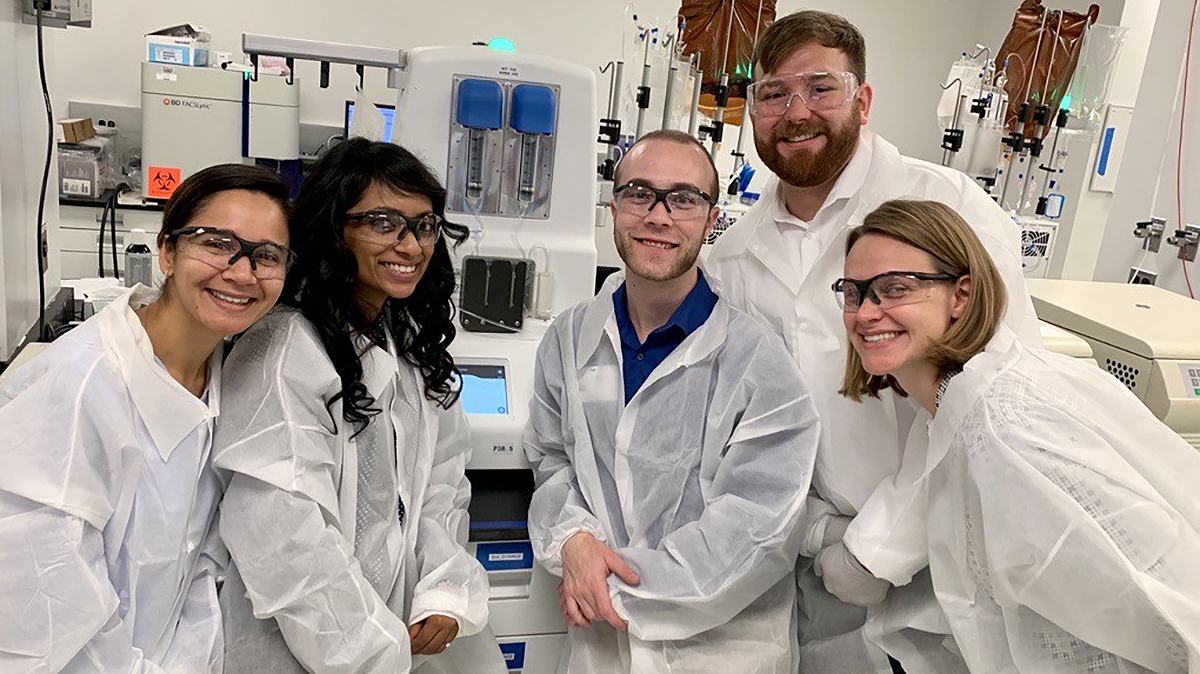
Fresenius Kabi's research team has been working on the Lovo and Cue cell processing systems for quite some time
For a long time, Fresenius Kabi has been supporting the use of CAR-T cell therapies: The company may not be directly involved in medical research into CAR-T cell therapies, but it does have a hand in manufacturing the technical laboratory equipment needed for it.
In the USA, for example, Fresenius Kabi is developing and producing two new devices that are essential to the CAR-T cell therapy process. A strong development team in Lake Zurich has been working on developing the automated Lovo Cell Processing System since 2016, under the aegis of Wegener. And since 2022, work has been continuing on the development of the Cue Cell Processing System. These devices are used in the complex manufacturing process for CAR-T cell therapy as a form of “production equipment.”
“We used to use a centralized R&D team for both the Lovo and the Cue development projects, meaning the colleagues switch to working on the projects as and when their expertise is required – sometimes supporting more than one project at a time,” explains Wegener. “At its peak, both the Lovo and Cue project team operated with around 35 colleagues.”
How it all began
The research community worldwide had started developing CAR-T processes back in 2011, nearly 15 years ago. “The initial processes employed to produce the specific cell cultures in a bioreactor were similar to the work performed in a medical research laboratory: Scientists moved around in special clean rooms, wearing the familiar “bunny suits” and using pipettes to transfer liquids between test tubes and flasks,” recalls Wegener, who originally studied biomedical engineering. “But after a while, when it transpired that the CAR-T cells worked astonishingly well for cell therapy, the researchers simply maintained this laborious, time-consuming approach.”
In order to be able to treat more patients, however, the production process would have to move into larger clean rooms and be performed on a larger scale. This expansion is known in technical jargon as a scale-out. “But after some time, you run out of qualified researchers, meaning that you then have a resource problem – and it becomes too expensive to build more clean rooms,” says Wegener. “Ultimately, at some point in the development, it is simply no longer possible to treat all patients who need therapy.” The developers of therapeutics had realized that they need to change fundamentally the way in which they produce CAR-T cells.

What is needed: Highly complex and automated devices
For the necessary expansion of the manufacturing process, two things in particular are important, according to Wegener: “Above all, highly complex and automated devices are needed that have been specially developed for the production processes associated with CAR T-cell therapy. And these systems must be self-contained – in other words, sterile,” Wegener continues. It turned out that the Lovo and Cue systems Kabi has been developing for more than eight years, meet precisely these requirements: They are automated to such an extent that even personnel who are less qualified can simultaneously carry out several processes. They are also flexible and can be configured to support many different workflows. And what’s more, the devices can be operated outside the clean room.
“We have thus taken a big step closer to bringing about the urgently needed expansion of the manufacturing process,” says Wegener on a positive note. “However, our Lovo and Cue systems cannot manage the entire process alone. Other instruments and processes must be put in place upstream and downstream of our systems,” explains Wegener.

Second development step: largely automated but in a central production facility
Even though the individual work stages are fully automated, the production of cell cultures is still generally carried out centrally, in one single processing facility. Despite all their complexity, such facilities can still produce high-quality therapeutic cells very reliably. However, such a central facility is usually not located anywhere near the patient.
The latest findings in the context of gene and cell therapy have shown that the widespread practice of running highly automated production processes in one central facility – far away from the patients – does not always make sense. Therefore, the research community and therapy developers are working hard to find new ways of simplifying the production process further. Effective and innovative solutions could point in a completely new direction and include decentralizing all of the processes involved in the production of cell cultures. This would bring production closer to the so-called “point of care” – in other words, to the bedside or rather the patient.
“And this is precisely where our focus of research into solutions and devices for the next generation of technology will lie,” says Dr. Marc-Alexander Mahl, President of Pharma, Nutrition and Sustainability at Fresenius Kabi. What’s more, the research is being conducted with the aim to significantly shorten the production process to less than a day or even just a few hours.
However, we expect special applications or conditions where the therapeutic production process at the point of care is not optimal. “It will therefore be important to develop in parallel lab process features for our Lovo and Cue cell processing systems and to further expand the existing product range,” adds Dr. Mahl.
Learn more about the opportunities and risks of this innovative treatment option in our interview with Prof. Bertram Glass, Chief Physician for Hematology and Stem Cell Therapy at Helios Hospital Berlin-Buch: CAR-T cell therapy: Innovative therapy with the aid of genetically modified cells
Contact
Fresenius Kabi AG
Else-Kröner-Straße 1
61352 Bad Homburg v.d.H
Germany
T +49 (0) 6172 686 0
communication@fresenius-kabi.com


